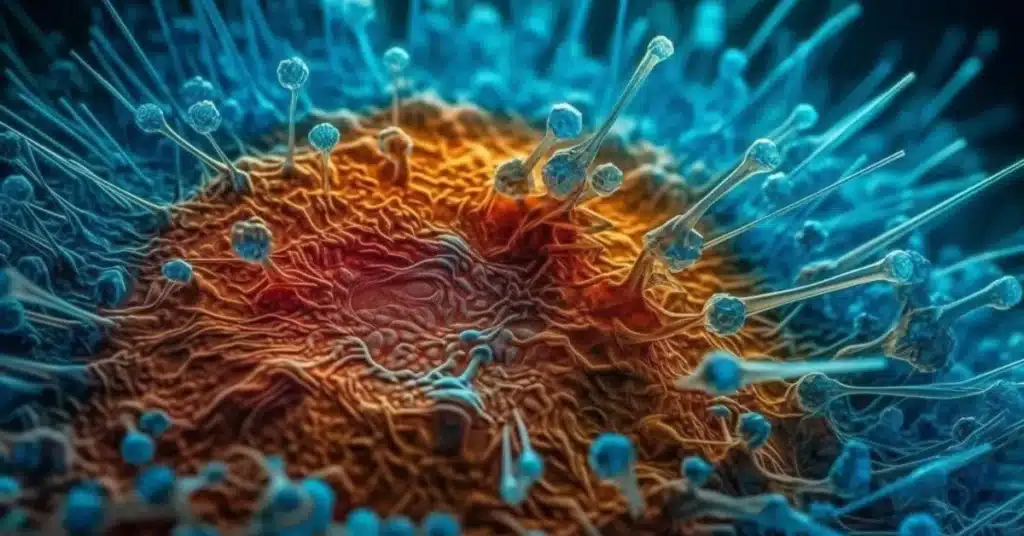
In a world where modern medicine has made great progress, a new adversary has emerged, threatening to undo decades of progress: superbugs. These tiny yet formidable foes pose a significant threat to human health, challenging our ability to treat common infections. From hospitals to communities, superbugs lurk, causing concern among healthcare professionals and public health experts alike.

In this article, we will know what is superbug. Why Are Superbugs Dangerous? and How Are Superbugs Created? By examining these aspects, we aim to gain a clear understanding of the topic.
Table of Contents
What are Superbugs?
Superbugs are strains of bacteria, viruses, fungi, or other microorganisms that have developed resistance to the drugs designed to kill them. They are often referred to as “super” because they possess extraordinary abilities to withstand antibiotics and other medications that were once effective against them. These resilient microbes can cause infections that are difficult, and sometimes impossible, to treat using conventional methods.
Read Similar: What is Oatzempic? Is Tiktok Oatzempic Weight Loss Drink Helps?
Why Are Superbugs Dangerous?
The danger of superbugs lies in their ability to render traditional treatments ineffective, leaving patients vulnerable to severe and potentially life-threatening infections. When antibiotics fail to combat these resistant microbes, illnesses can become prolonged, leading to increased suffering, hospitalizations, and even death.

One of the most alarming aspects of superbugs is their potential to spread rapidly within healthcare settings, such as hospitals and long-term care facilities. Patients with weakened immune systems are particularly susceptible to infections caused by these resilient pathogens, further complicating their medical care and recovery.
Moreover, the rise of superbugs undermines the effectiveness of essential medical procedures, such as surgeries, organ transplants, and cancer treatments, which rely heavily on the use of antibiotics to prevent and treat infections. Without effective antibiotics, these procedures become riskier, jeopardizing patient safety and overall healthcare outcomes.
How Are Superbugs Created?
Superbugs are not born resistant to antibiotics; rather, their resistance develops over time through various mechanisms. One common way superbugs emerge is through the misuse and overuse of antibiotics. When antibiotics are used unnecessarily or prescribed incorrectly, bacteria have the opportunity to adapt and evolve resistance mechanisms, allowing them to survive exposure to these drugs.
Furthermore, inadequate infection control measures in healthcare settings can facilitate the spread of resistant microbes from one patient to another. Poor sanitation practices, improper use of medical devices, and inadequate hand hygiene among healthcare workers can all contribute to the transmission of superbugs within hospitals and other healthcare facilities.
Additionally, the widespread use of antibiotics in agriculture, particularly in livestock farming, has been linked to the emergence of antibiotic-resistant bacteria in animals, which can then spread to humans through the food chain or environmental contamination.
How do fight superbug phages?
Fighting superbugs with phages involves using bacteriophages, which are viruses that specifically target and infect bacteria, as a form of therapy to combat antibiotic-resistant infections. Phage therapy harnesses the natural ability of bacteriophages to infect and kill bacteria, offering a promising alternative to traditional antibiotics in the treatment of multidrug-resistant bacterial infections.
Here’s how phage therapy works:
- Phage Isolation and Selection: Bacteriophages are isolated from various sources, such as sewage, soil, or environmental samples, based on their ability to target specific bacterial strains. Phages that demonstrate high specificity and efficacy against target bacteria are selected for further use in therapy.
- Phage Amplification: Once isolated, bacteriophages are cultured and amplified in the laboratory to increase their concentration and ensure sufficient quantities for therapeutic use. This step involves growing phages on bacterial host strains susceptible to their infection.
- Phage Administration: Phages can be administered to patients through various routes, including oral ingestion, topical application, or direct injection into the site of infection. Depending on the nature and location of the infection, phages may be administered individually or in combination with other treatment modalities.
- Phage-Bacterial Interaction: Upon administration, bacteriophages target and attach to specific receptors on the surface of bacterial cells, initiating the process of infection. Once attached, phages inject their genetic material into the bacterial cell, hijacking its machinery to replicate and produce progeny phages.
- Bacterial Cell Lysis: As phages replicate inside bacterial cells, they cause the host cell to undergo lysis, or bursting, releasing newly formed phage particles into the surrounding environment. This process leads to the destruction of bacterial cells and the subsequent reduction of the bacterial population.
- Immune Response: Following phage administration, the patient’s immune system may mount an immune response against both the infecting bacteria and the phages themselves. However, phages possess mechanisms to evade immune detection and clearance, allowing them to continue targeting and eliminating bacterial pathogens.
Phage therapy offers several potential advantages over traditional antibiotics in the treatment of antibiotic-resistant infections. These include:
- Specificity: Bacteriophages exhibit high specificity for their target bacteria, minimizing disruption to the normal microbial flora and reducing the risk of collateral damage to beneficial bacteria.
- Adaptability: Bacteriophages can rapidly evolve and adapt to changes in bacterial populations, making them potentially effective against emerging antibiotic-resistant strains.
- Biofilm Penetration: Phages have been shown to penetrate and disrupt bacterial biofilms, which are communities of bacteria encased in a protective matrix, making them particularly effective in treating chronic and persistent infections.
While phage therapy shows promise as an alternative approach to combatting antibiotic-resistant infections, several challenges and limitations exist, including the need for rigorous safety and efficacy testing, the development of standardized protocols for phage isolation and administration, and the potential for the emergence of phage-resistant bacterial strains.
Despite these challenges, ongoing research and clinical trials continue to explore the potential of phage therapy as a valuable tool in the fight against superbugs and antibiotic resistance. With further advancements in phage technology and a greater understanding of phage-bacterial interactions, phage therapy may offer new hope for patients facing untreatable bacterial infections.
The Role of CDC and the Latest Statistics
The Centers for Disease Control and Prevention (CDC), the leading national public health institute in the United States, closely monitors the threat of antibiotic resistance and works to address it through surveillance, research, and prevention efforts.
According to the CDC, antibiotic-resistant infections cause at least 2.8 million illnesses and 35,000 deaths each year in the United States alone. These infections result in significant healthcare costs and impose a substantial burden on patients and the healthcare system as a whole.
One concerning trend highlighted by the CDC is the rise of multidrug-resistant organisms (MDROs), which are capable of resisting multiple classes of antibiotics. These MDROs include notorious pathogens such as methicillin-resistant Staphylococcus aureus (MRSA), carbapenem-resistant Enterobacteriaceae (CRE), and extensively drug-resistant tuberculosis (XDR-TB), among others.
In addition to healthcare-associated infections, superbugs are increasingly being identified in community settings, posing a threat to otherwise healthy individuals outside of hospitals and healthcare facilities. This shift underscores the urgent need for comprehensive strategies to combat antibiotic resistance at both the local and global levels.

Combating the Threat of Superbugs
Addressing the threat of superbugs requires a multifaceted approach that encompasses healthcare practices, public education, research, and policy interventions. Key strategies recommended by the CDC and other public health agencies include:
- Antibiotic Stewardship: Promoting the judicious use of antibiotics in healthcare settings through evidence-based prescribing practices, antibiotic stewardship programs, and education for healthcare providers and patients.
- Infection Prevention and Control: Implementing robust infection control measures, such as hand hygiene protocols, environmental cleaning, and surveillance systems, to prevent the spread of resistant microbes in healthcare facilities.
- Research and Development: Investing in research to develop new antibiotics, diagnostics, and alternative treatments for antibiotic-resistant infections, as well as strategies to preserve the effectiveness of existing antibiotics.
- Global Collaboration: Collaborating with international partners to address antibiotic resistance on a global scale, sharing best practices, and coordinating efforts to combat the spread of superbugs across borders.
- Public Awareness: Raising awareness among the general public about the importance of responsible antibiotic use, infection prevention, and the threat posed by superbugs through education campaigns, community outreach, and media engagement.
Conclusion
Superbugs represent a significant public health challenge with far-reaching implications for healthcare delivery, patient outcomes, and global health security. Without urgent action to address antibiotic resistance, we risk entering a post-antibiotic era where common infections become untreatable, and essential medical interventions become perilous.
By implementing comprehensive strategies to combat superbugs and preserve the effectiveness of antibiotics, we can safeguard the health and well-being of current and future generations. Through collaboration, innovation, and sustained effort, we can overcome the threat of superbugs and ensure a safer, healthier future for all.
Frequently Asked Questions (FAQs)
What is the most common superbug in healthcare?
The most common superbug in healthcare settings is methicillin-resistant Staphylococcus aureus (MRSA). This bacterium can cause a wide range of infections, including skin and soft tissue infections, pneumonia, and bloodstream infections. MRSA is particularly concerning due to its resistance to multiple antibiotics, making treatment challenging.
How are superbugs cured?
Curing superbugs can be challenging due to their resistance to antibiotics. Treatment options may include using alternative antibiotics that the superbug is still susceptible to, employing combination therapy, or resorting to non-antibiotic treatments such as bacteriophage therapy or immunotherapy. However, successful treatment depends on the specific superbug and its level of resistance.
what causes superbugs?
Superbugs are primarily caused by the overuse and misuse of antibiotics. When antibiotics are used unnecessarily or prescribed incorrectly, bacteria have the opportunity to adapt and develop resistance mechanisms. Additionally, inadequate infection control measures in healthcare settings can contribute to the spread of resistant microbes, further fueling the emergence of superbugs.
what are superbug symptoms?
Superbug symptoms can vary depending on the type of infection and the specific microorganism involved. However, common symptoms of superbug infections may include fever, chills, pain or discomfort at the site of infection, inflammation, redness, and swelling. In more severe cases, symptoms may also include difficulty breathing, persistent cough, nausea, vomiting, diarrhea, and confusion. It is essential to seek medical attention if you experience any concerning symptoms, especially if you suspect a superbug infection.
What are superbugs and examples?
Superbugs are strains of bacteria, viruses, or other microorganisms that have developed resistance to antibiotics, making them difficult to treat. Examples include methicillin-resistant Staphylococcus aureus (MRSA), carbapenem-resistant Enterobacteriaceae (CRE), and multidrug-resistant tuberculosis (MDR-TB). These pathogens pose a significant threat to public health, as they can cause severe and sometimes untreatable infections, leading to increased morbidity and mortality.

