If you’re dealing with peripheral artery disease (PAD), you know how crucial it is to find the Best sleeping position for peripheral artery disease. PAD is a condition that affects blood flow to your limbs, particularly your legs, due to narrowed arteries. This restriction can lead to various symptoms like leg pain, cramping, and numbness, which can worsen during sleep. That’s why understanding the significance of sleep position is vital for PAD patients.
When we talk about the best sleeping position for peripheral artery disease, we’re aiming to optimize blood flow to the affected limbs while minimizing discomfort. Certain sleep positions can either alleviate or exacerbate PAD symptoms. For instance, sleeping on your back, known as the supine position, might not be the best choice for PAD patients as it can restrict blood flow to the legs, worsening symptoms like pain and numbness. On the other hand, side sleeping or elevating the legs can help improve circulation and reduce discomfort for individuals with PAD.
So, finding the best sleeping position for peripheral artery disease isn’t just about getting a good night’s sleep; it’s about managing symptoms and promoting better overall health. By choosing the right position, you can optimize blood flow to your limbs, alleviate discomfort, and improve the quality of your sleep, ultimately enhancing your quality of life.
1. Understanding Peripheral Artery Disease (PAD)
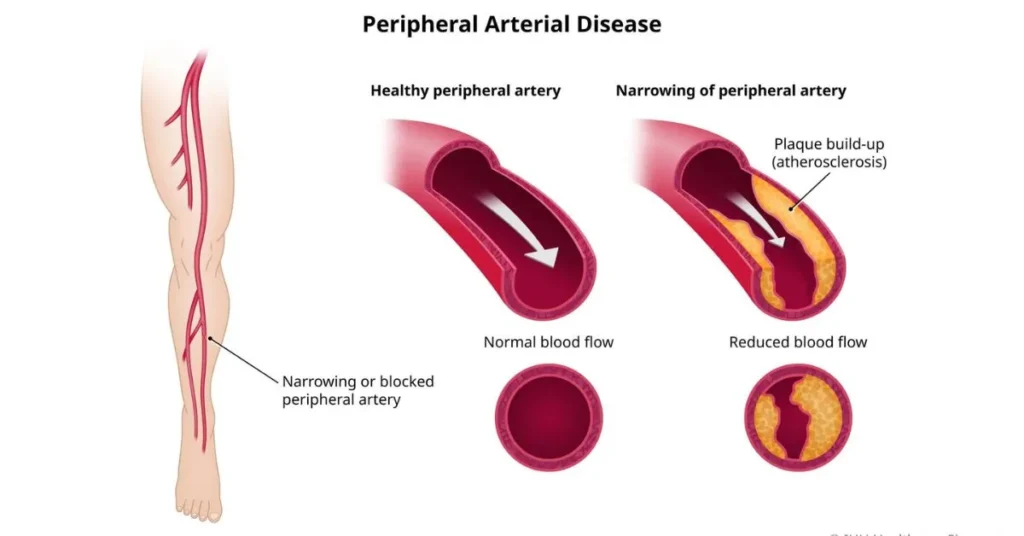
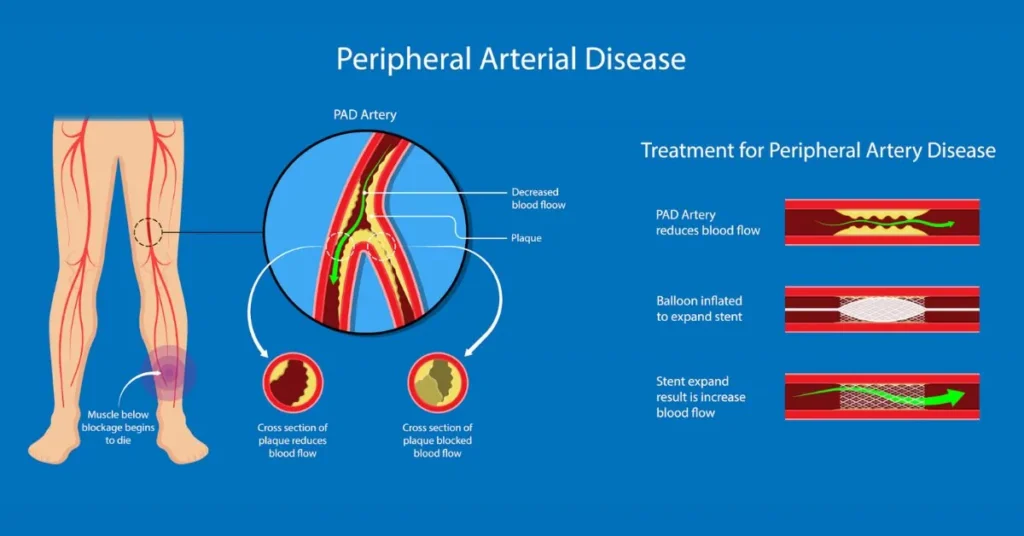
Peripheral Artery Disease (PAD) is a condition characterized by narrowed arteries, predominantly affecting the blood flow to the legs. This narrowing, often caused by atherosclerosis, a buildup of plaque in the arteries, restricts the flow of oxygen-rich blood to the limbs. Over time, PAD can lead to various complications due to reduced blood circulation.
What are the causes of peripheral artery disease
The primary cause of PAD is atherosclerosis, which occurs when fatty deposits, cholesterol, and other substances accumulate on the inner walls of the arteries. These deposits, known as plaques, can gradually narrow the arteries, restricting blood flow to the legs. Other factors that contribute to the development of PAD include:
Read More: What is Oatzempic? Is Tiktok Oatzempic Weight Loss Drink Helps?
- Smoking: Tobacco use damages the lining of the arteries, increasing the risk of plaque buildup.
- Diabetes: Individuals with diabetes are more prone to developing PAD due to elevated blood sugar levels that can damage blood vessels.
- High blood pressure (hypertension): Increased pressure within the arteries can lead to arterial damage and atherosclerosis.
- High cholesterol: Elevated levels of LDL cholesterol (often referred to as “bad” cholesterol) can contribute to the formation of plaques in the arteries.
- Sedentary lifestyle: Lack of regular physical activity can contribute to obesity, high blood pressure, and other risk factors for PAD.
Symptoms of Peripheral Artery Disease (PAD)
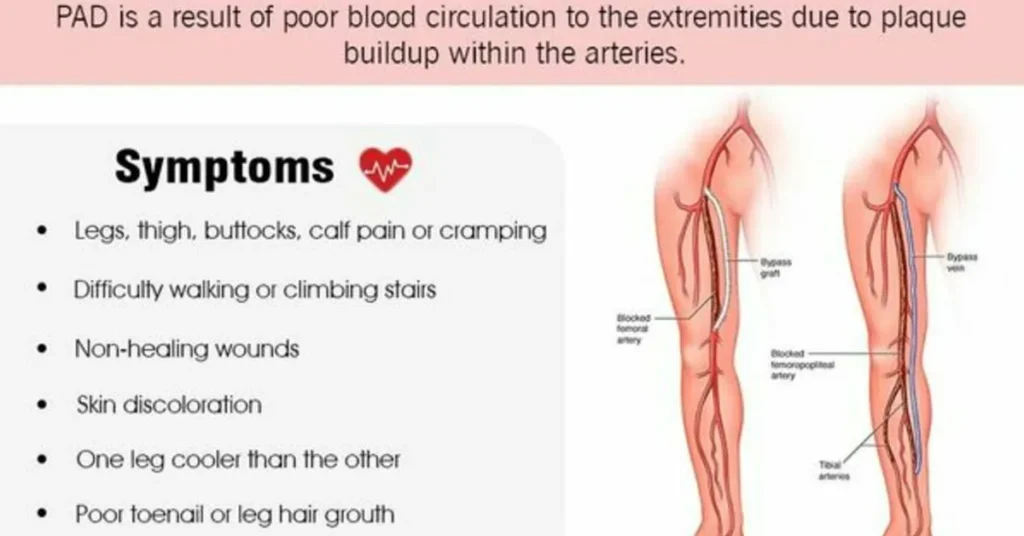
PAD often presents with symptoms related to reduced blood flow to the legs. Common symptoms include:
- Leg pain: Cramping, heaviness, or discomfort in the calves, thighs, or buttocks, particularly during physical activity (intermittent claudication).
- Numbness or weakness: Decreased sensation or muscle weakness in the legs, especially during movement.
- Coldness or discoloration: Cool or pale skin on the legs, often accompanied by changes in skin color or texture.
- Slow-healing wounds: Sores or ulcers on the legs or feet that heal slowly or do not heal properly.
- Poor nail and hair growth: Reduced growth of nails and hair on the legs and feet due to insufficient blood supply.
Risk Factors for PAD
Several factors increase the risk of developing PAD, including:
- Age: PAD is more common in individuals over the age of 50, although it can occur at any age.
- Smoking: Tobacco use is one of the most significant risk factors for PAD, increasing the likelihood of developing the condition and worsening its symptoms.
- Diabetes: People with diabetes are at higher risk of developing PAD due to elevated blood sugar levels that can damage blood vessels.
- High blood pressure: Hypertension can damage the arteries and increase the risk of atherosclerosis and PAD.
- High cholesterol: Elevated levels of LDL cholesterol and low levels of HDL cholesterol can contribute to plaque buildup in the arteries.
- Obesity: Excess weight puts additional strain on the circulatory system and increases the risk of atherosclerosis and PAD.
- Family history: Individuals with a family history of PAD or cardiovascular disease are at higher risk of developing the condition themselves.
Understanding the definition, causes, symptoms, and risk factors of PAD is essential for early detection, management, and prevention of complications. If you experience any symptoms of PAD or have risk factors for the condition, it’s crucial to consult a healthcare professional for evaluation and appropriate management.
2. The Link Between Sleep Position and PAD
The relationship between sleep position and Peripheral Artery Disease (PAD) is significant, as it directly impacts blood circulation and can affect the severity of PAD symptoms. Here’s how sleep position influences blood circulation and the impact of different positions on PAD symptoms:
How Sleep Position Affects Blood Circulation
The position in which you sleep can influence the distribution of blood throughout your body, including to the limbs affected by PAD. When you lie down, gravity plays a role in determining how efficiently blood flows to various parts of your body. Certain sleep positions can either enhance or impede blood circulation to the legs:
- Supine Position (Sleeping on Your Back): Sleeping on your back can potentially restrict blood flow to the legs, especially if your legs are not elevated. In this position, gravity may cause blood to pool in the lower extremities, exacerbating PAD symptoms such as leg pain and numbness.
- Side Sleeping: Side sleeping is generally considered beneficial for individuals with PAD, as it can improve blood circulation to the legs. By lying on your side, you reduce pressure on the blood vessels in the lower back and legs, allowing for better blood flow.
- Elevated Legs Position: Elevating your legs while sleeping can help facilitate blood circulation and alleviate symptoms of PAD. By raising your legs above the level of your heart, you promote venous return, allowing blood to flow more freely back to the heart and reducing swelling and discomfort in the legs.
Impact of Different Positions on PAD Symptoms
The choice of sleep position can significantly impact the severity of PAD symptoms experienced during sleep and upon waking. Here’s how different positions may affect PAD symptoms:

- Supine Position: Sleeping on your back without elevation may exacerbate symptoms such as leg pain, cramping, and numbness. The lack of elevation can lead to reduced blood flow to the legs, contributing to discomfort and restless sleep.
- Side Sleeping: Side sleeping is often recommended for individuals with PAD, as it can alleviate pressure on the blood vessels and improve blood circulation to the legs. This position may help reduce symptoms such as leg pain and numbness, promoting a more restful night’s sleep.
- Elevated Legs Position: Elevating your legs while sleeping can provide relief from symptoms of PAD by reducing swelling and improving blood flow. This position may help alleviate discomfort and promote better sleep quality for individuals with PAD, especially when combined with other supportive measures such as using pillows for elevation.
Overall, choosing the right sleep position is essential for individuals with PAD to manage symptoms and promote better circulation. While side sleeping and elevating the legs are generally recommended, it’s essential to find the position that is most comfortable and effective for you. Experimenting with different sleep positions and using supportive measures such as pillows can help optimize sleep quality and alleviate symptoms of PAD. If you experience persistent or worsening symptoms, consult a healthcare professional for personalized advice and treatment recommendations.
3. Best Sleeping Position for Peripheral Artery Disease
Finding the best sleeping position is crucial for individuals with Peripheral Artery Disease (PAD) to manage symptoms and promote better sleep quality. Here’s a breakdown of the recommended sleeping positions for PAD and their benefits:
a. Supine Position: Benefits and Drawbacks

The supine position, or sleeping on your back, is a common sleep posture that offers both benefits and drawbacks for individuals with PAD:
Benefits:
- Neutral spine alignment: Sleeping on your back allows for natural alignment of the spine, which can reduce strain on the back and neck.
- Even weight distribution: With the body evenly supported, there’s less pressure on specific areas, potentially reducing discomfort.
- Ease of breathing: Sleeping on your back may promote better airflow, which can benefit individuals with breathing difficulties.
Drawbacks:
- Restricted blood flow: The supine position can compress blood vessels in the lower back and legs, potentially reducing blood flow to the limbs.
- Exacerbation of PAD symptoms: Reduced blood flow to the legs can worsen symptoms such as leg pain, cramping, and numbness.
Discomfort: Some individuals may find sleeping on their back uncomfortable, especially if they experience difficulty breathing or snoring.
While the supine position may not be ideal for everyone with PAD, some individuals may find relief by elevating their legs slightly with pillows to improve blood flow.
b. Side Sleeping: Advantages and Considerations
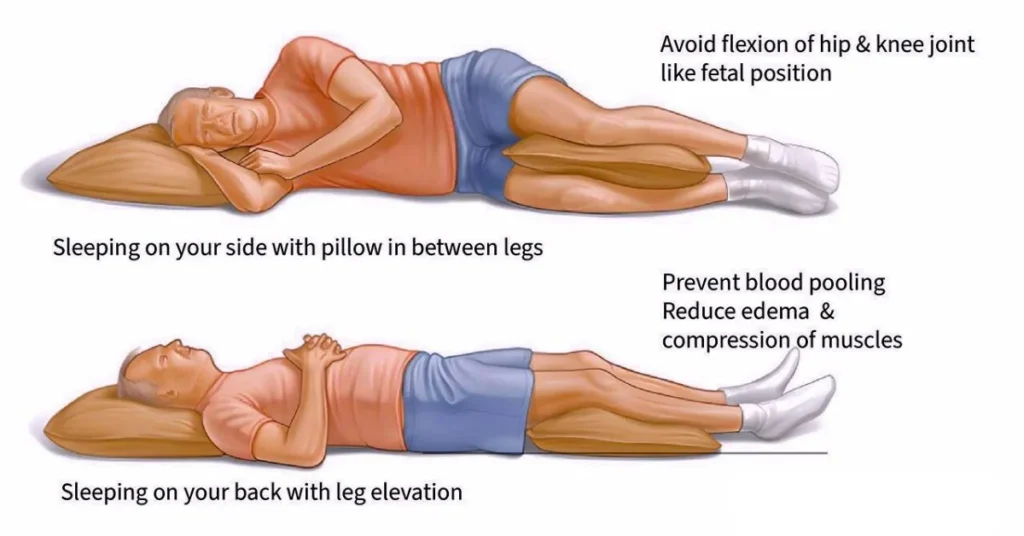
Side sleeping is often recommended for individuals with PAD due to its potential benefits for circulation and symptom management:
Advantages:
- Improved blood circulation: Side sleeping can enhance blood flow to the legs by reducing pressure on the blood vessels in the lower back and legs.
- Reduced pressure points: Sleeping on your side distributes weight more evenly, reducing pressure on specific areas of the body.
- Alleviation of symptoms: Many individuals find that side sleeping helps alleviate symptoms such as leg pain and numbness associated with PAD.
Considerations:
Proper alignment: It’s essential to maintain proper spinal alignment while side sleeping to prevent strain on the back and neck. Using a supportive pillow between the knees can help achieve alignment.
Comfort: Some individuals may find side sleeping uncomfortable, especially if they have shoulder or hip pain. Experimenting with pillow placement and mattress firmness can help improve comfort.
Overall, side sleeping is often considered one of the best sleeping positions for individuals with PAD due to its potential to improve circulation and alleviate symptoms.
c. Elevated Legs Position: Effectiveness for PAD Relief
Elevating the legs while sleeping can be an effective strategy for relieving symptoms of PAD and improving circulation:
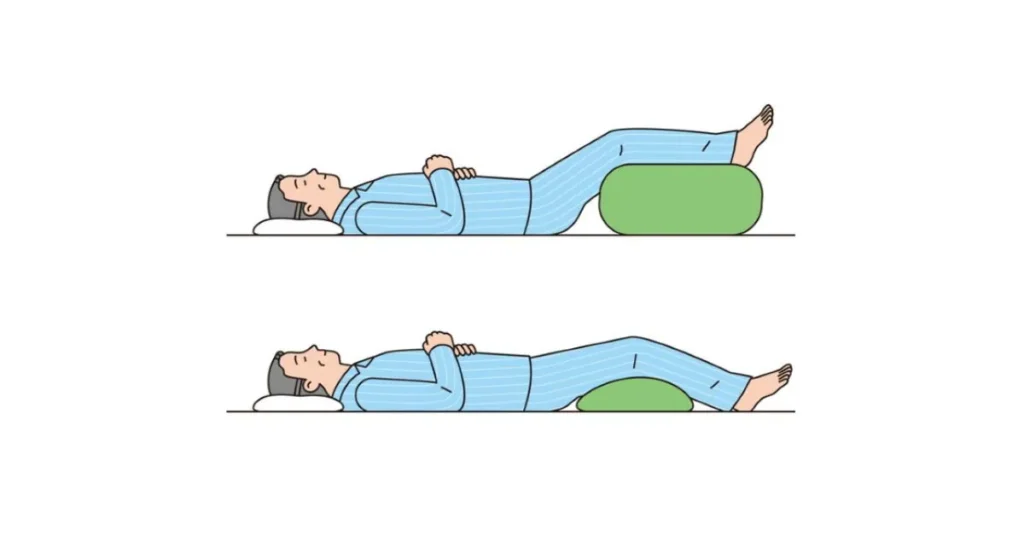
Effectiveness for PAD Relief:
- Improved blood flow: Elevating the legs above the level of the heart can promote venous return, helping blood flow more easily back to the heart and reducing swelling in the legs.
- Reduced pressure on blood vessels: By elevating the legs, you can alleviate pressure on the blood vessels in the lower extremities, potentially reducing discomfort and promoting better circulation.
- Alleviation of symptoms: Many individuals with PAD find relief from symptoms such as leg pain and swelling by elevating their legs while sleeping.
To achieve the elevated legs position, individuals can use pillows or a foam wedge to prop up their legs comfortably. It’s essential to ensure that the legs are elevated sufficiently to promote circulation without causing discomfort or strain.
In conclusion, the best sleeping position for individuals with PAD may vary depending on individual preferences and symptoms. While side sleeping and elevating the legs are generally recommended for improving circulation and alleviating symptoms, it’s essential to find the position that is most comfortable and effective for you. Experimenting with different sleeping positions and using supportive measures such as pillows can help optimize sleep quality and promote better overall health for individuals with PAD.
4. Tips for Comfortable Sleep with PAD
Ensuring a comfortable sleep environment is essential for individuals with Peripheral Artery Disease (PAD) to alleviate symptoms and promote restful sleep. Here are some tips for comfortable sleep with PAD:

Using Pillows for Support
Pillows can provide valuable support and help alleviate discomfort associated with PAD. Here’s how to use pillows effectively:
- Leg Elevation: Elevate your legs slightly using pillows to promote better blood flow and reduce swelling. Place pillows under your lower legs or feet to elevate them above the level of your heart.
- Knee Support: Place a pillow between your knees while side sleeping to align your spine properly and reduce strain on your hips and lower back.
- Neck Support: Use a supportive pillow that maintains proper alignment of your head and neck to prevent stiffness and discomfort.
Experiment with different pillow placements and firmness levels to find what works best for you and provides the most relief from PAD symptoms.
Adjusting Bedding and Mattress
Your bedding and mattress can significantly impact your sleep quality and comfort. Consider the following adjustments:
- Mattress Firmness: Choose a mattress with medium firmness that provides adequate support for your body while allowing for comfort. Avoid mattresses that are too firm, as they can increase pressure on sensitive areas.
- Bedding Material: Use soft, breathable bedding materials that promote airflow and temperature regulation. Opt for cotton or bamboo sheets and lightweight blankets to prevent overheating.
- Pillow Positioning: Ensure that your pillows are positioned correctly to support your head, neck, and spine in a neutral alignment. Avoid using too many pillows that can strain your neck or cause discomfort.
Regularly check your bedding and mattress for signs of wear and replace them as needed to maintain optimal comfort and support.
5. Temperature and Sleep Environment Considerations
Creating a conducive sleep environment can enhance your comfort and promote better sleep quality. Here are some considerations:

- Room Temperature: Keep your bedroom at a comfortable temperature, ideally between 60 to 67 degrees Fahrenheit (15 to 19 degrees Celsius), to promote relaxation and sleep. Use bedding layers that can be easily adjusted to accommodate temperature fluctuations.
- Noise Reduction: Minimize noise disruptions in your sleep environment by using earplugs, white noise machines, or soundproofing techniques. Ensure that your bedroom is quiet and conducive to restful sleep.
- Light Control: Create a dark sleep environment by using blackout curtains or blinds to block out light from windows. Limit exposure to electronic devices with blue light emissions before bedtime to promote natural sleep-wake cycles.
By implementing these tips for comfortable sleep with PAD, you can optimize your sleep environment and reduce discomfort, allowing for better rest and overall well-being. Experiment with different strategies to find what works best for you and prioritize quality sleep for improved health outcomes.
6. Other Lifestyle Changes to Improve PAD Symptoms
In addition to finding the best sleeping position, making lifestyle changes can significantly improve symptoms and overall well-being for individuals with Peripheral Artery Disease (PAD). Here are some recommendations for other lifestyle changes to consider:
Exercise Recommendations
Regular exercise plays a crucial role in managing PAD symptoms and improving circulation. Here are some exercise recommendations for individuals with PAD:
- Walking: Walking is a low-impact exercise that can improve blood flow to the legs and promote cardiovascular health. Start with short walks and gradually increase the duration and intensity as tolerated.
- Cycling: Cycling is another excellent exercise for individuals with PAD, as it provides a cardiovascular workout without putting excessive strain on the legs. Consider using a stationary bike or riding outdoors on flat terrain.
- Strength Training: Incorporating strength training exercises into your routine can help improve muscle strength and endurance, which can aid in walking and other daily activities. Focus on exercises that target the lower body, such as leg presses and calf raises.
- Flexibility Exercises: Stretching exercises can help improve flexibility and range of motion in the legs, reducing the risk of injury and enhancing overall mobility. Include stretches for the calves, hamstrings, and quadriceps in your exercise routine.
Consult with a healthcare professional or physical therapist before starting any exercise program, especially if you have existing health conditions or concerns about your ability to exercise safely.
Dietary Adjustments
Making dietary adjustments can support cardiovascular health and improve symptoms of PAD. Here are some dietary recommendations for individuals with PAD:
- Heart-Healthy Diet: Follow a heart-healthy diet that emphasizes fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit your intake of saturated and trans fats, cholesterol, and sodium.
- Omega-3 Fatty Acids: Include sources of omega-3 fatty acids in your diet, such as fatty fish (salmon, mackerel, sardines), flaxseeds, chia seeds, and walnuts. Omega-3 fatty acids have anti-inflammatory properties and may help improve circulation.
- Antioxidant-Rich Foods: Consume foods rich in antioxidants, such as berries, leafy greens, nuts, and seeds. Antioxidants help reduce inflammation and oxidative stress, which can benefit cardiovascular health.
- Hydration: Drink plenty of water throughout the day to stay hydrated and support optimal blood flow. Limit your intake of sugary beverages and alcohol, which can contribute to dehydration and negatively impact vascular health.

Smoking Cessation and Stress Management
Smoking cessation and stress management are essential components of PAD management. Here’s how to address these factors:
- Smoking Cessation: If you smoke, quitting is one of the most important steps you can take to improve your vascular health and reduce the progression of PAD. Seek support from healthcare professionals, quit-smoking programs, or support groups to increase your chances of success.
- Stress Management: Chronic stress can harm cardiovascular health and exacerbate PAD symptoms. Practice stress-reduction techniques such as deep breathing exercises, meditation, yoga, and spending time in nature. Engage in activities that promote relaxation and well-being, such as hobbies, spending time with loved ones, and enjoying leisure activities.
By incorporating these lifestyle changes into your daily routine, you can effectively manage symptoms of PAD, improve circulation, and enhance overall quality of life. Remember to consult with a healthcare professional for personalized recommendations and guidance on implementing these lifestyle changes safely and effectively.
7. Consulting a Healthcare Professional
Individuals with PAD need to consult with a healthcare professional for personalized advice and treatment recommendations. A healthcare provider can assess the severity of PAD, recommend appropriate lifestyle modifications, and prescribe medications or procedures to manage symptoms effectively. Additionally, they can offer guidance on optimizing sleep quality and finding the best sleeping position based on individual needs and preferences.
8. Conclusion
Finding the best sleeping position is essential for individuals with Peripheral Artery Disease to manage symptoms and promote better sleep quality. By understanding the relationship between sleep position and PAD, implementing supportive sleep habits, and making lifestyle modifications, PAD patients can experience improved comfort and overall well-being.