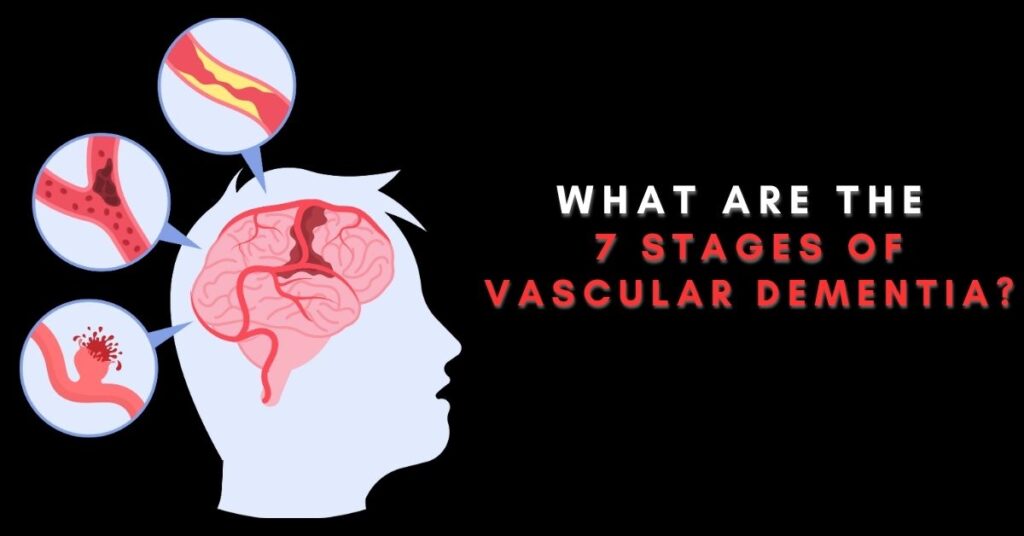
Vascular dementia is a type of dementia characterized by a decline in cognitive function due to reduced blood flow to the brain. It is the second most common form of dementia after Alzheimer’s disease. Understanding what vascular dementia is, its causes and risk factors is essential for managing the condition effectively and identifying the seven stages of vascular dementia.
1. What is Vascular Dementia?
Vascular dementia is a progressive neurological disorder caused by damage to the brain’s blood vessels. This damage impairs the brain’s ability to receive an adequate supply of oxygen and nutrients, leading to cognitive decline. Unlike other forms of dementia, which result from neurodegenerative processes, vascular dementia arises from cerebrovascular disease, including stroke, small vessel disease, and other conditions that affect blood flow to the brain.
Table of Contents
2. What are the types of vascular dementia?
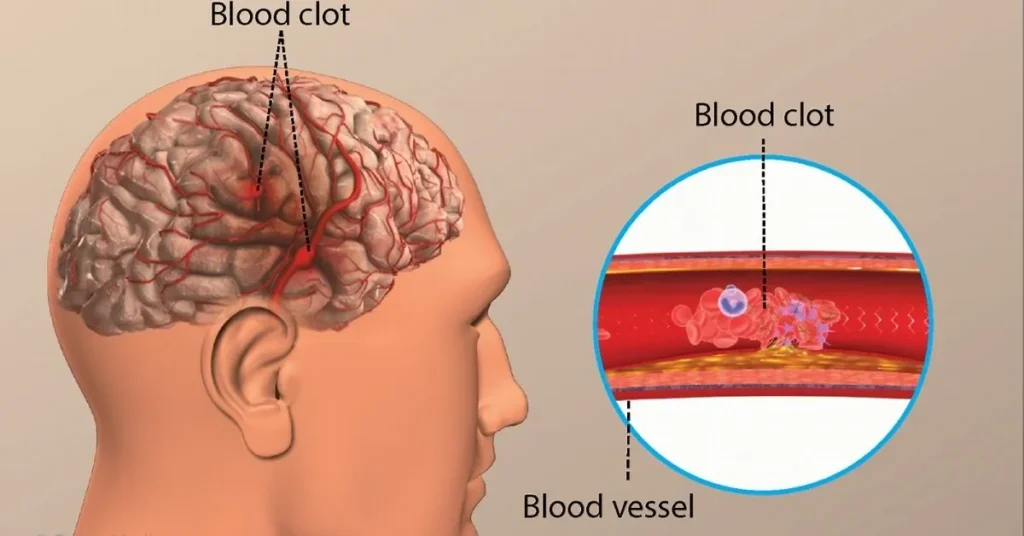
Vascular dementia happens when there are problems with blood flow to the brain. But why does this happen?
There are a few reasons why blood vessels might get damaged, leading to less blood flow to the brain. These reasons are like the “types” of vascular dementia.
Read More: Natural Remedies For Memory Loss in Menopause
The most common types are:
- Stroke-related dementia: This happens after a stroke when blood can’t get to the brain because of a clot.
- Multi-infarct dementia: This happens after many mini-strokes, or transient ischaemic attacks (TIA).
- Mixed dementia: This is when someone has symptoms of both vascular dementia and Alzheimer’s disease.
Vascular dementia can look different for each person depending on which part of the brain is affected.
For example, some people might forget things more often but can still do things on their own. Others might feel very confused or have trouble with balance.
Vascular dementia also gets worse differently for each person. It’s usually split into stages, which helps caregivers know what kind of care their loved one needs.
3. What is the difference between common dementia and vascular dementia?
Dementia is commonly described as a broad term encompassing symptoms such as memory loss, confusion, disorientation, and difficulties with judgment and planning. It’s important to note that dementia itself isn’t a disease; rather, it represents a cluster of symptoms associated with various underlying conditions.
There are numerous types of dementia, including the following:
- Alzheimer’s disease
- Vascular dementia
- Frontotemporal dementia
- Dementia with Lewy bodies
- Parkinson’s disease dementia
- Mixed dementia
- Huntington’s disease
- Creutzfeldt-Jakob disease
Each type can have different causes and treatments depending on where and how the brain is damaged.
Vascular dementia is one type of dementia caused by damage to the brain from reduced or blocked blood flow. Like other types of dementia, it can lead to memory problems and confusion, but the way it progresses and its early symptoms can be different because of the specific damage it causes.
Other types of dementia, like Alzheimer’s disease, are caused by abnormal proteins building up in the brain, forming plaques and tangles. Each type affects different parts of the brain and has its causes and symptoms.
4. What are the Causes and Risk Factors of Vascular Dementia?
Several factors contribute to the development of vascular dementia, including:
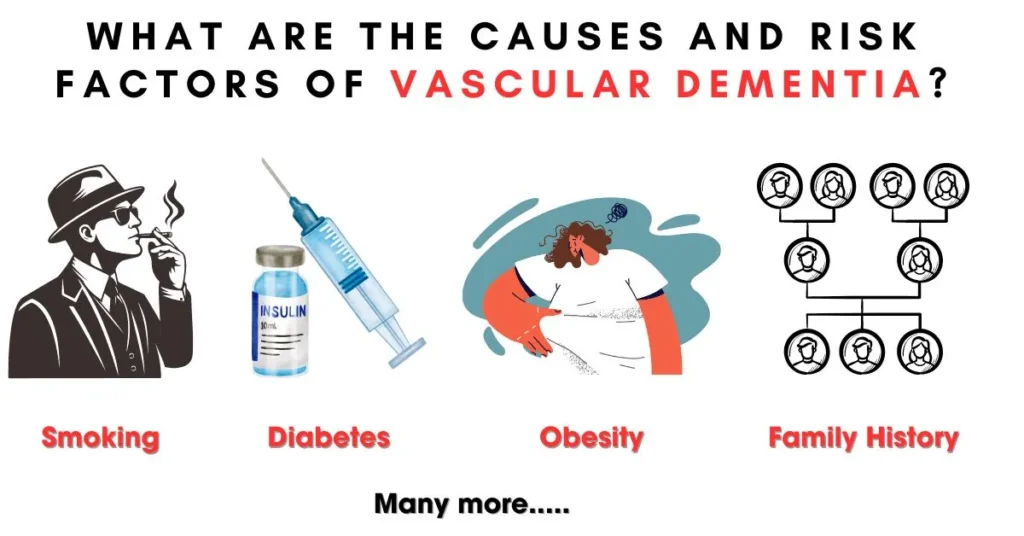
- Hypertension: High blood pressure increases the risk of damage to blood vessels in the brain, leading to vascular dementia.
- Diabetes: Uncontrolled diabetes can damage blood vessels throughout the body, including those in the brain, increasing the risk of cognitive impairment.
- Smoking: Tobacco use damages blood vessels and increases the risk of stroke and vascular dementia.
- Hypercholesterolemia: High levels of cholesterol can contribute to the buildup of plaque in blood vessels, restricting blood flow to the brain.
- Obesity: Excess weight is associated with an increased risk of cardiovascular disease and vascular dementia.
- Atrial Fibrillation: Irregular heart rhythm can lead to blood clots, increasing the risk of stroke and vascular dementia.
- Age: Advanced age is a significant risk factor for vascular dementia, with the risk increasing as individuals grow older.
- Family History: A family history of cerebrovascular disease or dementia may increase the risk of developing vascular dementia.
Understanding these causes and risk factors is essential for identifying individuals at risk of developing vascular dementia and implementing preventive measures to mitigate their impact. Early detection and intervention can help slow the progression of the disease and improve outcomes for individuals affected by it, highlighting the importance of knowing what the seven stages of vascular dementia are.
5. What are the 7 stages of vascular dementia? Explain With Symptoms
Stage 1: No Impairment
Description:
In Stage 1 of vascular dementia, individuals exhibit no signs of cognitive decline or impairment. This stage is characterized by normal brain function, where cognitive abilities such as memory, reasoning, and decision-making remain intact. There are no observable symptoms of vascular dementia during this phase, and individuals typically maintain their usual level of cognitive functioning.
Symptoms:
During Stage 1, individuals do not display any noticeable symptoms associated with vascular dementia. They can perform daily activities without difficulty and may not experience any changes in behavior or cognition. Memory, attention, and other cognitive functions are preserved, and there are no impairments in language or communication skills.
It’s important to note that while individuals may appear asymptomatic during Stage 1, they may still be at risk for developing vascular dementia later on. Regular monitoring of cognitive function and addressing any underlying risk factors, such as hypertension or diabetes, is essential for early detection and intervention.
Stage 2: Very Mild Decline
Description:
Stage 2 of vascular dementia marks the beginning of subtle changes in cognitive function. While still relatively mild, these changes may be noticeable to the individual or their close contacts. At this stage, cognitive impairment is minimal, but there may be occasional lapses in memory or cognitive performance. These changes are often subtle and may be attributed to normal aging or other factors.
Symptoms:
- During Stage 2, individuals may experience very mild cognitive decline, which can manifest as:
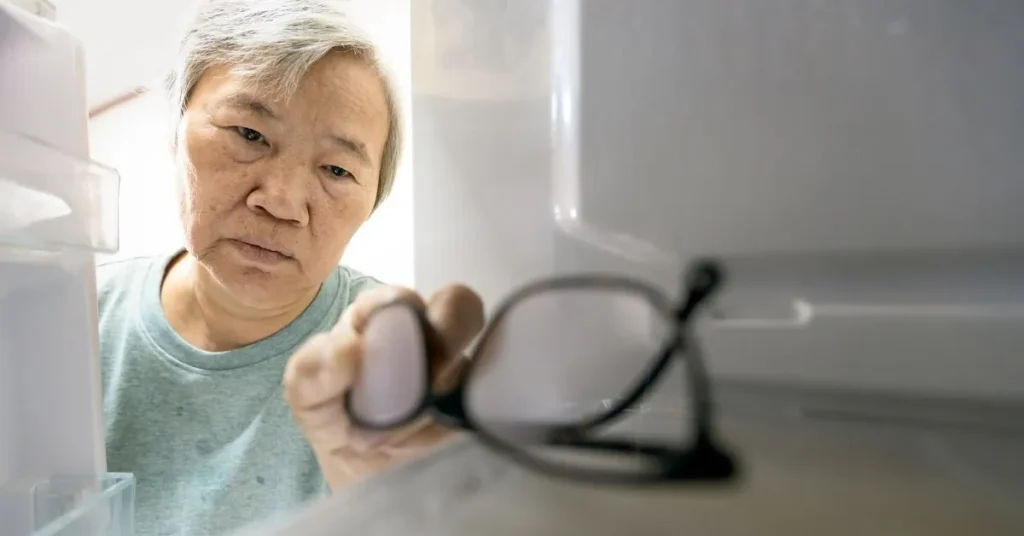
- Occasional forgetfulness, such as forgetting where they placed items or appointments
- Difficulty finding the right words or expressing thoughts
- Mild challenges with concentration or attention
- Slight changes in problem-solving abilities
These symptoms may not significantly impact daily functioning, and individuals can still carry out their usual activities independently. While these changes may be noticeable, they are often not severe enough to cause significant concern or impairment in daily life. However, it’s important to monitor these symptoms closely and seek medical evaluation if they persist or worsen over time. Early detection and intervention during Stage 2 can help individuals and their caregivers better manage the progression of vascular dementia.
Stage 3: Mild Decline
Description:
Stage 3 of vascular dementia represents a progression of cognitive decline beyond the very mild changes observed in Stage 2. At this stage, individuals may begin to experience more noticeable difficulties with cognitive function, which can impact daily activities and interactions. While still relatively mild compared to later stages, these changes may become more apparent to the individual and those around them.
Symptoms:
- During Stage 3, individuals with vascular dementia may exhibit the following symptoms:
- Increased forgetfulness, including difficulty remembering recent events or appointments
- Challenges with concentration and focus, lead to difficulty completing tasks
- Mild confusion, especially in unfamiliar or complex situations
- Difficulty with planning and organizing activities
- Changes in mood or behavior, such as increased irritability or apathy
These symptoms may become more evident to family members, friends, or caregivers, as they may notice changes in the individual’s behavior or abilities. While individuals with Stage 3 vascular dementia may still be able to perform many activities independently, they may require more assistance or support with tasks that involve higher levels of cognitive function. Caregivers and healthcare providers need to monitor these symptoms closely and provide appropriate support and intervention to help manage the progression of the disease.
Stage 4: Moderate Decline
Description:
Stage 4 of vascular dementia represents a significant progression in cognitive decline, with individuals experiencing moderate impairment in cognitive function. At this stage, the symptoms become more pronounced and may have a noticeable impact on the individual’s ability to perform daily activities independently.
Symptoms:
- During Stage 4, individuals with vascular dementia may exhibit the following symptoms:
- Increased memory impairment, including difficulty remembering recent events or familiar information
- Difficulty with language and communication, such as trouble finding the right words or following conversations
- Challenges with problem-solving and decision-making, leading to difficulties in planning and organizing tasks
- Impaired judgment, which may result in poor decision-making or risky behaviors
- Changes in behavior or personality, such as increased agitation, anxiety, or irritability
These symptoms may significantly affect the individual’s ability to function independently and may require assistance from caregivers or support services. While individuals in Stage 4 may still have some awareness of their condition, they may struggle to recognize the extent of their cognitive decline. Caregivers and healthcare providers must provide compassionate support and assistance to help individuals navigate the challenges of Stage 4 vascular dementia.
Stage 5: Moderately Severe Decline
Description:
Stage 5 of vascular dementia represents a significant advancement in cognitive decline, with individuals experiencing moderately severe impairment in cognitive function. At this stage, the symptoms become more pronounced and may significantly impact the individual’s ability to perform daily activities and maintain independence.
Symptoms:
- During Stage 5, individuals with vascular dementia may exhibit the following symptoms:
- Severe memory impairment, including difficulty remembering recent events, familiar faces, or important information
- Difficulty with language and communication, leading to challenges in expressing thoughts or understanding conversations
- Impaired executive function, resulting in difficulties with problem-solving, decision-making, and planning
- Reduced awareness of surroundings and changes in orientation, leading to disorientation and confusion
- Changes in behavior and mood, such as increased agitation, aggression, or withdrawal
These symptoms may require increasing levels of assistance and support from caregivers or healthcare professionals. Individuals in Stage 5 may struggle to perform basic activities of daily living independently and may require supervision or assistance with tasks such as dressing, bathing, and eating. Caregivers need to provide compassionate and patient care to help individuals maintain their dignity and quality of life during this challenging stage of vascular dementia.
Stage 6: Severe Decline
Description:
Stage 6 of vascular dementia represents a significant deterioration in cognitive function, with individuals experiencing severe impairment that greatly impacts their ability to perform daily activities. At this stage, individuals may require extensive assistance and support from caregivers to meet their basic needs.
Symptoms:
- During Stage 6, individuals with vascular dementia may exhibit the following symptoms:
- Severe memory loss, including an inability to recognize familiar faces or recall important personal information
- Profound difficulties with language and communication, with limited ability to speak or understand speech
- Impaired motor function, leading to difficulties with mobility and coordination
- Incontinence and other changes in bodily functions
- Behavioral symptoms such as agitation, aggression, or wandering
Individuals in Stage 6 may be unable to recognize their surroundings or communicate their needs effectively. They may require assistance with all activities of daily living, including eating, dressing, and personal hygiene. Caregivers play a crucial role in providing around-the-clock care and support to help individuals maintain comfort and dignity during this challenging stage of vascular dementia.
Stage 7: Very Severe Decline
Description:
Stage 7 of vascular dementia represents the most advanced and severe stage of cognitive decline. At this stage, individuals experience profound impairment in cognitive function, communication, and physical abilities. They require full-time care and support to meet their basic needs.
Symptoms:
- During Stage 7, individuals with vascular dementia may exhibit the following symptoms:
- Complete loss of verbal communication abilities, with limited or no ability to speak or understand speech
- Severe memory loss, including an inability to recognize even close family members or recall any personal information
- Loss of motor function and mobility, leading to dependence on others for all activities of daily living
- Incontinence and other changes in bodily functions, requiring assistance with toileting and personal hygiene
- Loss of awareness of surroundings and self, with minimal responsiveness to external stimuli
Individuals in Stage 7 are typically bedridden and may require specialized care in a hospice or palliative care setting. They are at high risk of developing complications such as infections or pressure ulcers due to immobility and impaired immune function. Caregivers provide compassionate end-of-life care, focusing on comfort and dignity for individuals in this final stage of vascular dementia.
6. What to expect in early-stage vascular dementia?
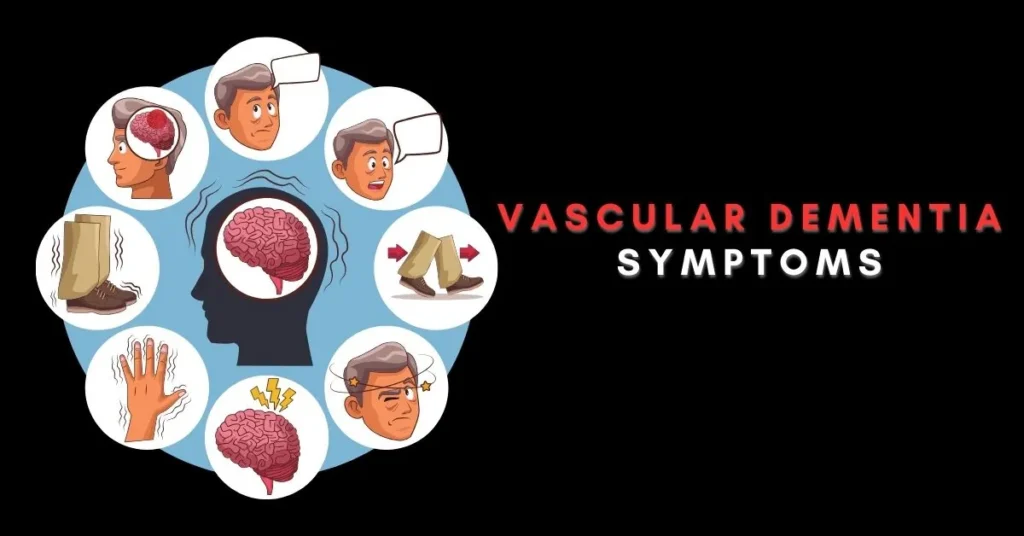
In the early stages of vascular dementia, damage to blood vessels or disruption of blood flow to the brain may have already happened, but symptoms are usually mild.

Unlike Alzheimer’s disease, where memory loss is often the first noticeable sign of cognitive decline, vascular dementia might show different signs at the start. People with vascular dementia might have more confusion, communication problems, and difficulty making decisions, planning, or solving problems.
During the early stages, it’s a good time to start planning for your loved one’s care because they can still be involved in the decisions.
It’s hard to say exactly how long the first stage of dementia lasts because changes in the brain happen for years before symptoms show up. However, each stage of dementia usually lasts around two years on average. But everyone progresses differently because many factors are involved.
7. What to expect in middle-stage vascular dementia?
During the middle stages of dementia, you can expect your loved one’s symptoms to progress.
They may start to show changes in behavior, increased confusion, and difficulties with communication.
Symptoms of depression and anxiety might also appear as your loved one deals with moderate cognitive decline, loss of independence, and frustration with communication.
As these changes occur, your loved one will need more care, emotional support, and understanding.
At this stage, it might be a good idea to consider additional in-home care or moving to an assisted living community with memory care.
The Kensington White Plains offers two memory care communities tailored to meet your loved one’s specific needs. We provide a comprehensive life enrichment program and various onsite services to help residents engage in social, physical, and wellness activities, maintaining their quality of life to the fullest.
8. What to expect in late-stage vascular dementia?
In the later stages of dementia, your loved one will need significant help with their daily activities like eating, dressing, and using the bathroom.
The final stage of dementia is usually the shortest, lasting about one to two years.
During this time, the focus is on keeping your loved one comfortable, maintaining a routine, and engaging their senses.
Understanding your loved one’s nonverbal cues and finding ways to communicate with them become crucial as verbal communication may become limited.
At any stage of dementia, it’s important to highlight what the person can still do rather than focusing on what they’ve lost.
Establishing a routine can provide comfort, and surrounding them with familiar things like old photos, favorite movies, games, and music can help.
At The Kensington White Plains, we offer various programs such as cognitive-stimulating activities, music therapy, pet therapy, robo-pets, and pocket programming to promote connection and reduce anxiety among our residents.
9. How do you prevent vascular dementia?
Improving your overall health and well-being can help prevent or reduce the symptoms of vascular dementia.

This involves:
- Engaging in regular exercise
- Avoiding smoking and excessive alcohol consumption
- Properly managing existing health conditions like high blood pressure or diabetes
It also includes following a heart-healthy and brain-healthy diet, such as the MIND diet. This diet emphasizes foods like green leafy vegetables, whole grains, nuts, berries, and healthy fats, which can support brain health and reduce the risk of cognitive decline.
10. Factors Affecting Progression
Medical Intervention:
Effective medical intervention plays a crucial role in managing the progression of vascular dementia. Early diagnosis and treatment of underlying conditions such as hypertension, diabetes, and high cholesterol can help reduce the risk of further cognitive decline. Additionally, medications may be prescribed to manage symptoms such as memory loss, agitation, and mood changes. Regular monitoring by healthcare professionals allows for adjustments to treatment plans as needed, optimizing outcomes for individuals with vascular dementia.

Lifestyle Changes:
Adopting healthy lifestyle habits can also positively impact the progression of vascular dementia. Engaging in regular physical activity promotes cardiovascular health and can help improve blood flow to the brain. Following a balanced diet rich in fruits, vegetables, whole grains, and lean proteins provides essential nutrients that support brain function. Avoiding smoking and excessive alcohol consumption reduces the risk of vascular damage and cognitive decline. Furthermore, staying socially active and mentally stimulated through hobbies, socializing, and cognitive exercises can help preserve cognitive function and enhance overall well-being. By incorporating these lifestyle changes, individuals with vascular dementia can potentially slow the progression of the disease and improve their quality of life.
11. How to Care and Support for Individuals with Vascular Dementia
Importance of Support:
Support for individuals with vascular dementia is essential for ensuring their well-being and quality of life throughout the progression of the disease. As cognitive function declines, individuals may struggle to perform daily activities independently and may experience emotional challenges such as confusion, frustration, and anxiety. Providing compassionate care and support helps individuals feel valued, respected, and understood, fostering a sense of dignity and security during this challenging time. Additionally, support from caregivers and healthcare professionals plays a vital role in addressing the diverse needs of individuals with vascular dementia, including physical, emotional, and social aspects of care.

Strategies for Caregivers:
Caregivers of individuals with vascular dementia require access to effective strategies and resources to provide optimal care and support. Some strategies for caregivers include:
- Education and Information: Educating caregivers about the progression of vascular dementia, common symptoms, and effective caregiving techniques helps them better understand and respond to the needs of their loved ones.
- Communication: Effective communication with individuals with vascular dementia involves using simple, clear language, maintaining eye contact, and practicing patience and empathy. Listening attentively and validating their feelings and experiences can enhance communication and foster trust and connection.
- Routine and Structure: Establishing a consistent daily routine and structured environment can help individuals with vascular dementia feel more secure and oriented. Providing clear instructions and cues for daily activities can reduce confusion and agitation.
- Safety Measures: Implementing safety measures such as removing hazards from the environment, installing grab bars and handrails, and using assistive devices can prevent accidents and injuries and promote independence and mobility.
- Self-Care: Caregivers must prioritize their well-being to effectively support individuals with vascular dementia. Taking regular breaks, seeking respite care, and accessing support groups or counseling services can help caregivers manage stress, prevent burnout, and maintain their own physical and emotional health.
By implementing these strategies and accessing support resources, caregivers can enhance the quality of life for individuals with vascular dementia and provide compassionate and effective care throughout the progression of the disease.
12. Conclusion
In summary, vascular dementia progresses through seven stages, each characterized by unique symptoms and challenges.
Stage 1 marks the absence of cognitive decline, while Stage 2 represents very mild changes. Stage 3 signifies mild decline, progressing to Stage 4 where moderate impairment becomes evident. Stage 5 sees a moderately severe decline, followed by Stage 6 which indicates severe impairment. Finally, Stage 7 represents the most advanced and severe decline.
Early detection and intervention are crucial in managing vascular dementia effectively. Recognizing the signs and symptoms early allows for timely medical evaluation and intervention, which can help slow the progression of the disease and improve outcomes for individuals affected by it. By implementing appropriate treatments, lifestyle modifications, and supportive care, individuals with vascular dementia can maintain their quality of life and independence for as long as possible.
Ultimately, a comprehensive approach that includes medical management, lifestyle changes, and supportive care is essential in addressing the complex needs of individuals with vascular dementia and enhancing their overall well-being. Early detection and intervention play a pivotal role in optimizing outcomes and improving the lives of those affected by this condition.
13. Frequently Asked Questions (FAQ’s)
How is vascular dementia diagnosed?
Vascular dementia is typically diagnosed through a combination of medical history, physical examination, cognitive tests, brain imaging, and blood tests.
Can vascular dementia be prevented?
While it may not be possible to prevent vascular dementia entirely, adopting a healthy lifestyle, managing underlying medical conditions, and staying mentally and physically active can help reduce the risk.
What treatments are available for vascular dementia?
Treatment for vascular dementia focuses on managing symptoms, preventing further cognitive decline, and addressing underlying vascular risk factors. Medications, lifestyle changes, and supportive therapies may be recommended.
What is the difference between vascular dementia and Alzheimer’s disease?
Vascular dementia is caused by reduced blood flow to the brain, often as a result of stroke or small vessel disease, whereas Alzheimer’s disease is characterized by the accumulation of abnormal proteins in the brain.
How does vascular dementia affect daily life?
Vascular dementia can impact various aspects of daily life, including memory, communication, decision-making, and mobility. As the disease progresses, individuals may require increasing levels of assistance with everyday tasks.